Experimental Drug Restores Chemical Balance In The Brain And May Transform PTSD Treatment
- Lidi Garcia
- Aug 4
- 5 min read

Scientists have discovered that people with PTSD have an imbalance in a substance called GABA in the brain, caused by cells called astrocytes. This excess GABA makes it difficult to overcome fear and persists with symptoms of the disorder. A new drug, KDS2010, has restored this balance in animal trials and has shown safety in humans, paving the way for a new, more effective way to treat PTSD.
Post-traumatic stress disorder, known as PTSD, is a serious mental condition that can arise after a person experiences an intense traumatic experience, such as an accident, abuse, war, or violence.
People with PTSD often experience disturbing thoughts that arise unexpectedly, try to avoid situations that remind them of the trauma, feel constantly on alert, and have difficulty controlling their emotions when faced with these memories. Despite the severity of the condition, available treatments are limited.
Currently, only two medications that act on serotonin, a brain chemical, are approved to treat PTSD. However, these medications only work fully in about 20 to 30 percent of patients. This clearly highlights the urgent need to develop new, more effective treatments.

An area of the brain called the prefrontal cortex (PFC) plays a fundamental role in how we cope with fear and overcome traumatic experiences.
Two specific parts of this region, called the prelimbic and infralimbic regions, help "turn off" or reduce the learned fear response, which is essential for recovery after trauma.
In people with PTSD, this ability to "turn off" fear appears to be compromised. Furthermore, their brains exhibit changes in a substance called GABA, which acts as a natural brake on brain activity, helping to calm and control nerve signals. When this brake malfunctions in the prefrontal cortex, the brain has more difficulty "unlearning" fear, which worsens PTSD symptoms.
Studies using advanced technologies, such as magnetic resonance spectroscopy, indicate that there are changes in GABA levels in people with PTSD. These changes appear to affect blood flow to the brain and contribute to the condition.
Another postmortem brain imaging study confirmed that GABA function in the brains of people with PTSD was dysregulated. Specifically, a brain cell called an astrocyte, previously thought to be merely a "helper" for neurons, is overproducing GABA through an enzyme called MAOB.

Under normal circumstances, astrocytes regulate GABA production to maintain balance, but under stress or disease, these astrocytes become "reactive," excessively increasing this production and disrupting the functioning of synapses (the connections between neurons).
This excessive production of GABA by astrocytes has been observed in other brain diseases, such as Alzheimer's, Parkinson's, and epilepsy, suggesting that it may be a common mechanism of brain dysregulation. In the case of PTSD, researchers suspect that this "toxic" GABA makes it even more difficult to overcome fear and contributes to the disorder's persistent symptoms.
To investigate this hypothesis, scientists conducted a large study with several approaches: they examined PTSD patients, analyzed human brains after death, and also tested mouse models that mimic PTSD behavior.
These studies confirmed that GABA levels were altered in the prefrontal region of the brains of people with PTSD and that this was linked to symptom severity. Furthermore, when scientists blocked the MAOB enzyme (responsible for the overproduction of GABA in astrocytes), the symptoms of excessive fear and difficulty "forgetting" the trauma were alleviated in mice.
A drug called KDS2010, which safely and selectively inhibits this enzyme, has shown encouraging results. It not only reduced excess GABA and improved brain function, but also successfully passed initial human trials (Phase 1) without causing serious side effects.
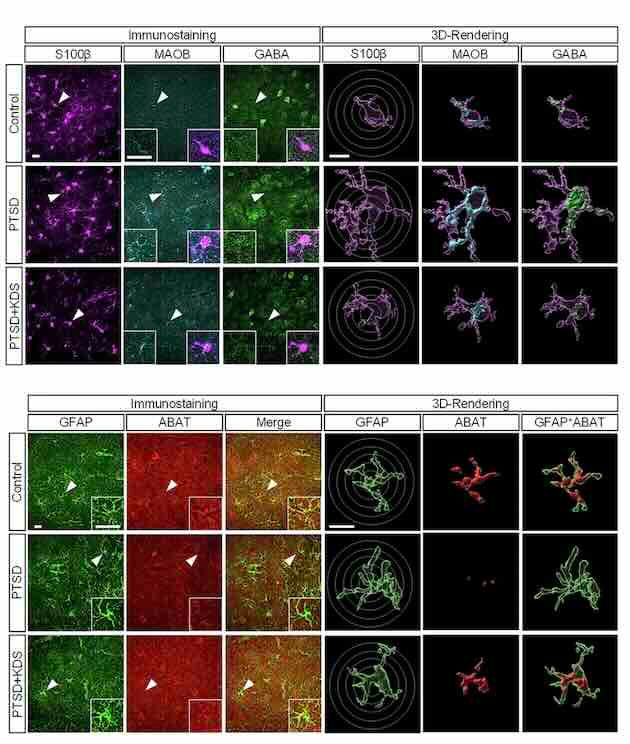
A study of a mouse model of control and PTSD treated with KDS2010. These images also compare the three groups: control, PTSD, and PTSD treated with KDS2010. The images shown were obtained using confocal microscopy (a technique that allows for the visualization of very small structures within the brain with high clarity) and Imaris software, which helps analyze these images in 3D. They show the presence of three chemical markers: S100β, which identifies astrocytes (a type of brain cell); MAOB, an enzyme that helps in the production of GABA; GABA, a neurotransmitter that inhibits brain activity (and which is altered in PTSD); GFAP, another marker of astrocytes, especially those that are reactive (i.e., activated by some type of damage or stress); ABAT, an enzyme that breaks down GABA and is also involved in brain chemical balance. The circle marks an analysis called Sholl, which measures the complexity of astrocytes by observing how many "arms" or branches they have, something that changes when these cells become "sick" or hyperactive.
Therefore, KDS2010 presents itself as a new and promising treatment option for PTSD. It acts directly on the mechanism of the problem, the GABA imbalance caused by reactive astrocytes, and not just on the symptoms.

Representative traces of tonic GABA currents across all groups.
This type of approach could pave the way for more effective treatments, offering hope to millions of people living with this debilitating disorder.
This research represents an important step in the search for therapies based on how the brain actually works (neurobiological mechanisms), connecting human studies, laboratory experiments, and the development of real drugs.
READ MORE:
Astrocytic gamma-aminobutyric acid dysregulation as a therapeutic target for posttraumatic stress disorder
Sujung Yoon, Woojin Won, Suji Lee, Kayoung Han, Eunji Ha, Juheon Lee, Seung Jae Hyeon, Yoonji Joo, Haejin Hong, Hyangwon Lee, Yumi Song, Ki Duk Park, Bertrand R. Huber, Junghee Lee, Richard A. E. Edden, Minah Suh, Hoon Ryu, C. Justin Lee, and In Kyoon Lyoo
Signal Transduction and Targeted Therapy, 10, Article number: 240 (2025)
DOI: 10.1038/s41392-025-02317-5
Abstract:
Post-traumatic stress disorder (PTSD) remains a debilitating psychiatric condition with limited pharmacological treatment options. Identifying novel therapeutic targets is critical for addressing its unmet clinical needs. Through our comprehensive human clinical research, including both cross-sectional and longitudinal studies, we revealed a compelling link between dysregulated prefrontal gamma-aminobutyric acid (GABA) levels and PTSD symptoms. Notably, elevated prefrontal GABA levels in PTSD patients are associated with impaired cerebral blood flow (CBF) and symptom severity, normalizing with recovery, highlighting GABA dysregulation as a key mechanism in the disorder. Postmortem and PTSD-like mouse models implicated monoamine oxidase B (MAOB)-dependent astrocytic GABA as a primary driver of this imbalance, exacerbating deficit in fear extinction retrieval. Genetic and pharmacological inhibition of MAOB effectively restored astrocytic GABA and improved fear extinction retrieval in PTSD-like mouse models. Specifically, KDS2010, a recently developed highly selective and reversible MAOB inhibitor, not only restored astrocytic GABA homeostasis but also rescued CBF deficits and reduced tonic GABA and astrogliosis in the prefrontal cortex. Moreover, KDS2010 successfully advanced through Phase 1 clinical trials, showing a favorable safety profile and paving the way for Phase 2 trials to evaluate its therapeutic potential in PTSD. Our findings highlight the pivotal role of astrocytic GABA in PTSD pathophysiology and establish MAOB inhibition as a mechanistically targeted approach to alleviate symptoms. By bridging human and animal studies with translational clinical trials, this work positions KDS2010 as a promising first-in-class therapy, offering a novel paradigm for PTSD treatment.



Comments